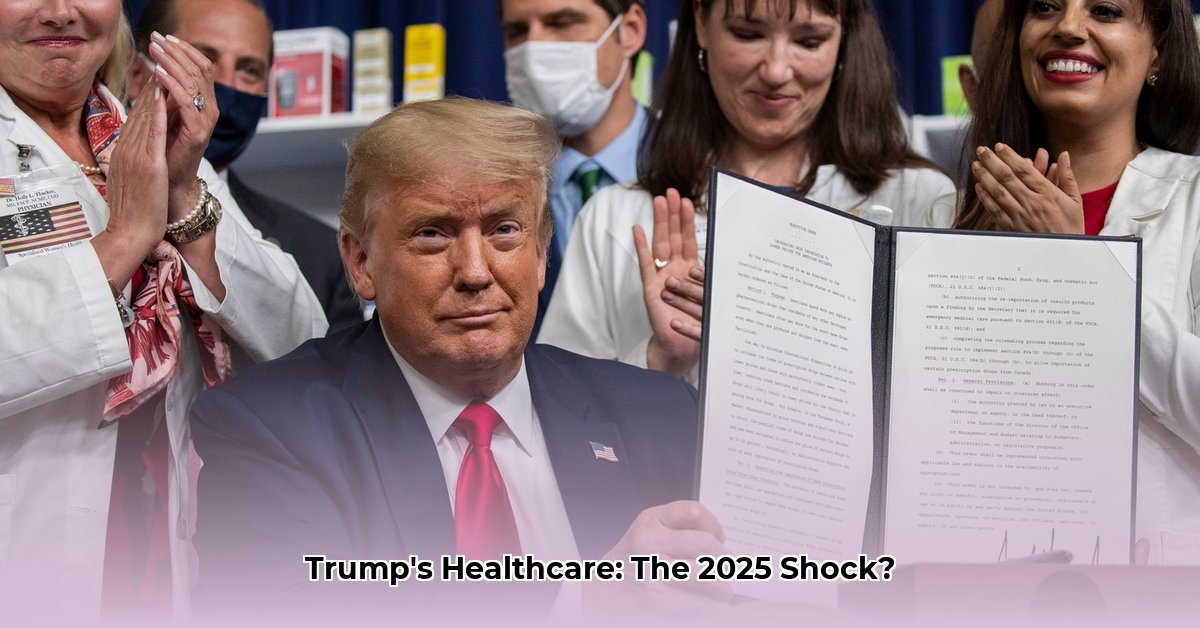
President Trump’s time in office significantly altered the healthcare landscape. This article analyzes the lasting effects of his policies as we approach 2025, comparing initial goals with actual outcomes. We examine deregulation efforts, highlighting both benefits and drawbacks. Expert insights provide a clear understanding of these complex changes. For further insights on healthcare policy, see [this analysis](https://www.lolaapp.com/patrick-soon/). Finally, we offer practical advice for navigating today’s healthcare environment and planning for the future, helping you stay informed and prepared.
Trump Healthcare: Unpacking the 2025 Impact and Long-Term Effects
Let’s analyze the long term impact of the Trump administration’s healthcare policies, focusing on their potential effects by 2025. The aim is to understand the complexities of these changes and their implications for patients, providers, and the healthcare system as a whole through healthcare initiatives.
Deregulation and Tight Budgets: The Core of Trump’s Healthcare Vision
A central tenet of President Trump’s healthcare strategy involved diminishing government oversight and implementing stricter budget controls. This translated to fewer federal regulations on programs like Medicaid and the Affordable Care Act (ACA), specifically impacting subsidies designed to help individuals afford health insurance. Consequently, states faced increased financial pressures. The intended outcome was heightened efficiency and cost reduction, yet the actual results present a mixed picture. Did these measures truly cut costs and improve efficiency concerning healthcare access, or did they inadvertently create new challenges?
Prescription Drug Pricing: An Unclear Landscape
The Trump administration aimed to introduce greater transparency in prescription drug prices. However, the overall success remains ambiguous. While certain Biden-era initiatives aimed at lowering drug costs were reversed, the long-term implications—particularly regarding Medicare’s capacity to negotiate drug prices—are uncertain. This suggests the administration had a strategy, balancing campaign promises with the potential for political repercussions.
Access to Healthcare: A Central Point of Debate
A major point of contention revolves around the effect of these policies on access to affordable healthcare. Many health advocates feared that cuts in public health funding would limit access and increase the number of uninsured Americans. Supporters argued that the cuts were vital for controlling government spending and eliminating waste. This difference in viewpoints complicates the matter. What is really happening in the long term across the country?
Healthcare Complexities: An Interplay of Factors
The Trump administration’s healthcare strategy wasn’t straightforward, with each decision leading to immediate outcomes. It involved political realities, economic pressures, and dynamics within the healthcare industry. The administration balanced fiscal responsibility with the popularity of existing programs like Medicare. Giving states more control added complexity. With state-level differences, healthcare access became uneven.
Pharmaceutical companies and pharmacy benefit managers (PBMs) also significantly impacted the results of these changes. Was there true transparency as intended? The interplay of these factors shapes the landscape of healthcare in 2025.
Stakeholders: Winners and Losers
This table summarizes the impact on various groups, looking at both short-term (within the first year) and long-term (three to five years) effects:
| Stakeholders | Short-Term (0-1 Year) | Long-Term (3-5 Years) |
|---|---|---|
| Healthcare Providers | Focused on efficiency improvements to adjust to budget cuts. | Adapted business strategies within a more competitive, less regulated market. |
| Insurance Companies | Adjusted pricing to reflect regulatory changes. | Navigated a more fragmented system. |
| Patients | Noticed changes in coverage and costs. | Experienced varying levels of access to care; individual advocacy became crucial. |
| Pharmaceutical Firms | Managed fluctuating revenue to potential drug price changes. | Adjusted to pricing pressures and changing market demands. |
| Government Agencies | Worked within budget limits and implemented price transparency initiatives. | Addressed emerging challenges and evaluated the results of decentralization. |
Potential Risks: Analyzing the Downsides
Analyzing potential consequences requires acknowledging several key risks:
| Risk Category | Likelihood | Impact | Possible Solutions |
|---|---|---|---|
| Medicaid Funding Cuts | High | Very High | Strategic planning and improved program efficiency. |
| ACA Subsidy Changes | High | High | Prepare for increased demand; increase support for at-risk populations. |
| Unclear Drug Pricing | Medium | Medium | Adapt to market shifts, diversify revenue, and monitor policy changes closely. |
In conclusion, the Trump administration’s healthcare changes were complex and had far-reaching consequences on the healthcare system. The push for less regulation and reduced spending created both opportunities and risks, especially regarding affordable healthcare access. The long-term effects are still unfolding, making ongoing analysis crucial. The future of American healthcare remains dynamic and constantly changing.
How did Trump’s healthcare deregulation impact state Medicaid programs?
Key Takeaways:
- Proposed Medicaid cuts aimed to slash hundreds of billions of dollars from the program’s funding over a decade, resulting in vulnerable populations at risk.
- Work requirements are affecting low-income individuals and those with disabilities.
- The actual impact varied across states, influenced by existing Medicaid expansion programs, state funding levels, and administrative capacities.
- Critics argued the cuts would severely reduce healthcare access for millions, exacerbating health disparities, however, proponents countered that the changes promoted fiscal responsibility and individual accountability.
- Legal challenges added to the uncertainty surrounding the overall impact.
The Trump administration’s approach to healthcare, with deregulation and Medicaid cuts, changed state Medicaid programs. Let’s look at the key changes and results and impacts of Medicaid.
Changes: Funding Reductions and Work Requirements
The most significant changes were from proposed federal funding cuts and work requirements for Medicaid recipients. These aimed to cut spending and encourage personal responsibility.
The reality was more nuanced. While the financial impact varied by state, reports showed enrollment declines, especially among vulnerable groups. The work requirements created bureaucratic hurdles, making it hard for eligible people to keep coverage. Did this really help or hurt people that needed the most help?
State-Level Impact: Responses and Infrastructure
How did Trump’s healthcare deregulation impact state Medicaid programs in different ways? It depended on each state’s infrastructure and budget priorities. States with Medicaid expansion programs struggled with funding shortfalls, forcing tough choices about service provision. Other states, already implementing work requirements, saw the enforcement challenges and the social cost of individuals losing healthcare coverage.
This shows this decentralized American healthcare system. The federal government’s Medicaid changes created state-level responses, creating access inconsistencies across the nation.
For instance, some states re-allocated funding or created alternative programs. Others struggled with increased uninsured individuals, straining existing healthcare resources. For example, Kentucky’s attempt to implement work requirements was challenged in court, highlighting the legal and administrative complexities involved 1.
Consequences: Unintended Effects and Ongoing Debates
The ripple effects extended beyond enrollment. Rural hospitals, already struggling financially, faced reduced reimbursements and more uninsured patients. The impact on public health, debated during the policy’s implementation, is being studied. Will increased rates of uninsured people lead to more preventable deaths? Did the work requirements truly improve employment statistics? These require long-term analysis.
Lessons: Future Challenges
The Trump administration’s Medicaid overhaul offers lessons about healthcare policy complexities. Deregulation, while intended to improve efficiency and reduce spending, can have significant consequences. The experience highlights understanding federal regulations and state-level implementation. Continued research is crucial for understanding the long-term effects on health and well-being.
Trump Healthcare Deregulation Efforts: State-Level Impacts and Challenges
Key Takeaways:
- The Trump administration’s healthcare policies shifted power to the states significantly, leading to a patchwork of healthcare regulations.
- Deregulation aimed to boost market efficiency and lower costs but sparked concerns about patient access and healthcare quality.
- The impact on vulnerable populations remains a key area of debate.
- AI’s rapid adoption in healthcare under deregulation presents novel challenges.
- The long-term effects of these changes, especially on the financial health of the system and equitable access, are uncertain.
Unpacking: Deregulation and Healthcare in America
The Trump administration’s approach to healthcare was marked by deregulation. This altered the relationship between the federal government and individual states in managing healthcare. Did this decentralization lead to efficiency gains, or did it create new problems? The administration’s actions, through executive orders and regulatory rollbacks, created a complex situation.
Impact: Assessing Winners and Losers
Some argue reduced federal oversight fostered innovation and competition, potentially lowering healthcare costs for some. Others express deep concerns about the vulnerable populations. They point to potential consequences for those who might lose access to essential services due to weakened regulations and reduced funding. This includes concerns about reduced federal oversight of Medicaid and the potential for increased health disparities.
Patchwork: State-Level Scramble
The shift to state control resulted in a fragmented healthcare system. States gained flexibility in designing their healthcare programs, leading to a wide range of approaches and outcomes [2]. Some states embraced innovation, while others struggled to maintain existing levels of coverage and care.
The inconsistencies pose challenges for patients, providers, and insurers operating across state lines. Navigating this fragmented landscape requires a deep understanding of state-specific regulations and policies.
Technology: AI and Telehealth
Deregulation also influenced the adoption of new technologies, such as AI
- Uncover Verna Garver’s historical significance: A biography - July 20, 2025
- Uncover Verna Garver’s Untold Story: A Life Beyond Hollywood - July 20, 2025
- Uncovering Verna Garver’s Cause of Death: A Biography - July 20, 2025











1 thought on “Trump Healthcare Overhaul: 2025 Impact Analysis”
Comments are closed.