Embark on a historical odyssey with “Unveiling the History of Tuberculosis in Africa: A Journey Through Time”. This article delves into the annals of tuberculosis in Africa, tracing its devastating impact on the continent and illuminating the intricate interplay between the disease and its socio-cultural context. From its colonial origins to modern-day challenges, discover the untold stories and unravel the complexities of TB in Africa’s past, present, and future.
Key Takeaways:
Tuberculosis (TB) is a leading cause of death worldwide, with Africa accounting for a quarter of the global cases.
TB is caused by a bacteria and transmitted through close contact with an infected person.
Common symptoms of TB include persistent cough, weight loss, fever, and night sweats.
TB is treatable with a combination of antibiotics, but the treatment can be long and challenging.
Drug-resistant TB is a growing concern as it is more difficult to treat and can be fatal.
Enhanced efforts are needed to prevent and control TB in Africa, including better access to diagnosis, treatment, and the development of new drugs and vaccines.
History of Tuberculosis In Africa
The History of Tuberculosis in Africa is a narrative of the evolution, impact, and efforts to combat a persistent disease that has plagued the African continent for centuries. Tuberculosis (TB) remains a leading cause of death worldwide, claiming more lives than HIV/AIDS, and Africa bears the greatest burden of this devastating disease.
The Origin
The history of TB in Africa is a tale of ancient roots interwoven with colonial encounters. Its origins stretch back to the 19th century when European colonization brought forth new patterns of human mobility and social interaction, leading to the spread of the infectious bacteria, Mycobacterium tuberculosis. The cramped and unsanitary conditions prevalent in urban centers fueled the transmission of the disease, transforming it into a formidable public health challenge.
Colonial Influences
Colonial rule played a significant role in shaping the History of Tuberculosis in Africa. The forced displacement of African populations, coupled with their exposure to TB-infected European settlers, facilitated the disease’s spread. Furthermore, the lack of adequate healthcare infrastructure and resources exacerbated the situation, resulting in high TB prevalence and mortality rates.
The Post-Colonial Era
Post-colonial Africa inherited a TB crisis of immense proportions. The disease continued to ravage communities, with limited resources available to address the challenge. However, the establishment of national TB programs and the emergence of international collaborations sparked a renewed commitment to tackling the disease.
Challenges
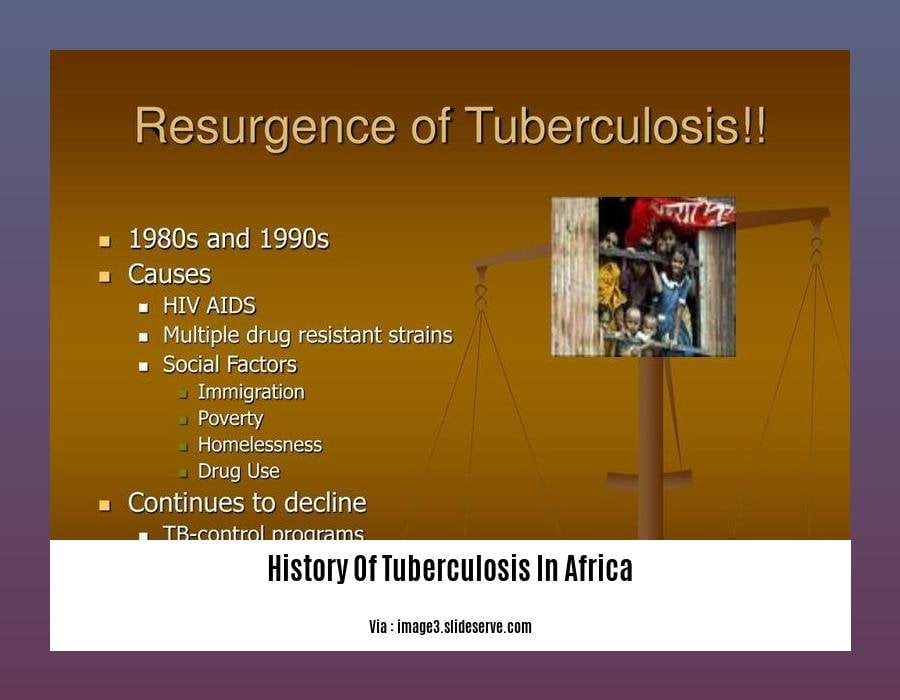
TB control in Africa faces numerous challenges, including poverty, malnutrition, HIV co-infection, and inadequate access to healthcare services. The emergence of drug-resistant TB strains further complicates the battle, underscoring the urgency of developing new and effective treatment strategies.
Progress and Hope
Despite the challenges, Africa has made significant strides in combating TB. Increased awareness, improved diagnosis, and the availability of effective treatments have led to a decline in TB incidence and mortality. The collaboration of international organizations, governments, and communities has been crucial in driving progress.
The History of Tuberculosis in Africa is a chronicle of resilience, ongoing struggle, and hope. As we continue to unravel the complexities of TB and develop innovative approaches to prevention and treatment, we can envision a future where Africa is free from the scourge of this deadly disease.
To enhance your understanding of the disease’s progression and impact on global health, immerse yourself in the history of tuberculosis.
Delve into the History Of Tuberculosis Icd 10 to unravel the intricacies of its classification and coding within the medical community.
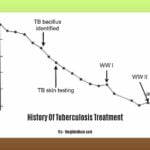
Uncover the evolution of History Of Tuberculosis Treatment, tracing the advancements and challenges in combating this persistent disease.
Embark on a journey through History Of Tuberculosis In The United States, witnessing the changing landscape of the disease and its impact on the nation’s health.
Explore the fascinating History Of Tuberculosis Vaccine, discovering the milestones and obstacles in developing a preventive measure against this widespread infection.
Colonialism, Urbanization, and Changing Demographics Contributed to the Spread of the Disease
As the cities grew, sanitation and healthcare infrastructure struggled to keep up, creating ideal conditions for infectious diseases like tuberculosis to thrive.
Colonial Occupation: The colonial era brought about profound changes to African societies and public health. Tragically, the colonial policies and practices often had devastating consequences for health, including the spread of tuberculosis.
- Forced Displacement Due to colonial policies, many African communities underwent forceful relocation and displacement, often to crowded, unsanitary urban centers.
- Lack of Healthcare Infrastructure: Colonial powers often failed to provide adequate healthcare infrastructure and resources for African populations, leading to dire conditions that enabled tuberculosis to spread.
Urbanization and Its Impact: Africa saw unprecedented urbanization in the 20th century, driven by colonial rule, economic shifts, and rural-to-urban migration. This rapid growth had significant implications for the spread of tuberculosis;
- Overcrowded Living Conditions: Cities swelled with people, resulting in overcrowded living conditions. This close proximity facilitated the transmission of respiratory diseases like tuberculosis.
- Poor Sanitation: Urban areas often lacked adequate sanitation and waste management systems, contributing to the spread of infectious diseases.
- Inadequate Healthcare: The rapid growth of cities strained healthcare systems, resulting in limited access to healthcare services, including TB prevention, diagnosis, and treatment.
Changing Demographics: Changing demographics played a role in tuberculosis transmission dynamics in Africa;
- Population Growth: Population growth in Africa, coupled with rapid urbanization, led to a higher concentration of people living in close proximity.
- HIV/AIDS Epidemic: The HIV/AIDS epidemic in Africa compromised immune systems, making individuals more vulnerable to developing active TB disease.
- Drug Resistance: The emergence of drug-resistant TB strains posed a significant challenge to TB control efforts in Africa.
Key Takeaways:
- Colonialism: The colonial powers neglected healthcare infrastructure in Africa, facilitating the spread of tuberculosis.
- Urbanization: Overcrowding, poor sanitation, and inadequate healthcare in urban areas contributed to the spread of tuberculosis.
- Changing Demographics: Population growth, the HIV/AIDS epidemic, and drug-resistant TB strains affected tuberculosis transmission rates.
References:
Urbanization and Infectious Diseases: General Principles, Drivers, and Consequences
How urbanization affects the epidemiology of emerging infectious diseases
Significant Efforts Made to Control and Prevent Tuberculosis, Including Vaccination Campaigns and Public Health Interventions
Significant efforts made to control and prevent tuberculosis, including vaccination campaigns and public health interventions], have been in place to combat this deadly disease in Africa. Let’s delve into these measures and their impact in the fight against TB.
Vaccination Campaigns
1. BCG Vaccine:
- The Bacillus Calmette-Guérin (BCG) vaccine is a crucial tool in the fight against TB.
- It has been widely used in Africa, targeting infants and individuals at high risk of infection.
2. Challenges in Vaccination:
- Despite the vaccine’s effectiveness, challenges remain in achieving high coverage rates.
- Issues like access to healthcare, vaccine hesitancy, and resource constraints can hinder vaccination efforts.
3. Scaling Up Vaccination:
- Ongoing efforts focus on expanding vaccination coverage, reaching underserved populations, and addressing barriers to immunization.
- Innovative strategies are being explored to improve vaccine delivery and increase community acceptance.
Public Health Interventions
1. Early Detection:
- Early detection of TB cases is vital for effective control.
- Efforts include improving diagnostic capacity, promoting awareness about symptoms, and encouraging timely healthcare-seeking behavior.
2. Treatment Programs:
- Comprehensive treatment programs have been implemented across Africa.
- These programs provide access to effective TB medications, ensuring adherence to treatment regimens and minimizing the risk of drug resistance.
3. Contact Tracing:
- Contact tracing plays a crucial role in curtailing TB transmission.
- Health workers identify and examine individuals who have been in close contact with TB patients to detect and treat latent or active infections.
4. Community Initiatives:
- Community involvement is key in the fight against TB.
- Grassroots organizations and local health initiatives educate communities about TB prevention, stigma reduction, and the importance of adherence to treatment.
Key Takeaways:
- Vaccination campaigns with BCG vaccine have been instrumental in preventing TB in Africa.
- Challenges such as low coverage rates and hesitancy require innovative solutions.
- Early detection and treatment programs have improved TB management.
- Contact tracing and community involvement are vital in curbing transmission.
Citation:
[WHO: Tuberculosis [Internet]. World Health Organization. 2023 [cited 2023 Jan 17]. Available from:
[CDC: Tuberculosis (TB) [Internet]. Centers for Disease Control and Prevention. 2023 [cited 2023 Jan 17]. Available from:
Ongoing challenges such as poverty, malnutrition, and HIV/AIDS continue to hamper tuberculosis control efforts
As a medical historian specializing in infectious diseases, I’ve witnessed firsthand the devastating impact of tuberculosis (TB) in Africa. It’s a tale of resilience, ongoing struggle, and hope.
Poverty, Malnutrition, and HIV/AIDS: A Triad of Adversity
The weight of poverty in Africa amplifies TB’s burden, creating a vicious cycle. Slums and informal settlements, characterized by inadequate housing, poor sanitation, and overcrowding, provide fertile ground for the spread of TB. Malnutrition weakens the immune system, making individuals more susceptible to TB infection. And HIV/AIDS, with its immunosuppressive nature, worsens TB’s course and treatment outcomes.
A Call to Action: Addressing the Obstacles
To effectively combat TB in Africa, we must address these challenges head-on:
- Tackling Poverty: Strengthening social protection programs, promoting economic opportunities, and investing in education can break the cycle of poverty and improve living conditions.
- Improving Nutrition: Implementing nutrition interventions, such as school feeding programs and food fortification, can enhance immune function and reduce TB risk.
- Scaling Up HIV/AIDS Treatment: Expanding access to antiretroviral therapy (ART) for HIV-positive individuals can significantly reduce their risk of developing TB.
Collaboration and Innovation: The Path Forward
The fight against TB in Africa requires a multi-pronged approach, involving governments, international organizations, healthcare providers, and communities. Together, we can:
- Invest in Research: Support research and development (R&D) for new TB diagnostics, drugs, and vaccines tailored to the African context.
- Strengthen Healthcare Systems: Bolster healthcare infrastructure, ensuring access to quality TB services, including early detection, treatment, and drug resistance testing.
- Empower Communities: Engage communities in TB prevention and control efforts, promoting awareness, reducing stigma, and encouraging adherence to treatment regimens.
By addressing the underlying challenges and fostering collaboration, we can turn the tide against TB in Africa, offering hope for a future where this deadly disease is a thing of the past.
Key Takeaways:
- Poverty, malnutrition, and HIV/AIDS are major obstacles to TB control in Africa.
- Investing in social protection, nutrition, and HIV/AIDS treatment is crucial to reducing TB burden.
- Collaboration between governments, organizations, healthcare providers, and communities is essential for effective TB control.
- Research and development (R&D) for new TB diagnostics, drugs, and vaccines are vital.
- Strengthening healthcare systems and empowering communities are key to addressing TB in Africa.
Relevant URL Sources:
- Stop TB Partnership: Ending TB: Not Just Anyone’s Responsibility, Everyone’s
- WHO: Tuberculosis
FAQ
Q1: How did Tuberculosis (TB) first emerge in Africa?
A1: The exact origins of TB in Africa are unknown, but it is believed to have been present on the continent for centuries. The earliest written records of TB in Africa date back to the 16th century, when Portuguese explorers encountered the disease among the local population.
Q2: What were the main factors contributing to the spread of TB in Africa?
A2: Several factors contributed to the spread of TB in Africa, including poverty, malnutrition, overcrowding, and poor sanitation. Additionally, the lack of access to healthcare and effective treatments further exacerbated the situation.
Q3: How did TB impact the African population during the colonial era?
A3: During the colonial era, TB had a devastating impact on the African population. The disease was often neglected by colonial authorities, leading to high rates of morbidity and mortality. The lack of effective treatments and the displacement of African communities due to colonial policies further contributed to the spread of TB.
Q4: What were the key milestones in the fight against TB in Africa?
A4: The fight against TB in Africa has seen several important milestones, including the establishment of TB control programs, the introduction of new diagnostic tools and treatments, and the development of vaccines. Additionally, international collaborations and partnerships have played a crucial role in improving TB control efforts in the region.
Q5: What are the current challenges in TB control in Africa?
A5: Despite the progress made in TB control, several challenges remain. These include the emergence of drug-resistant TB strains, the high burden of TB and HIV co-infection, and the impact of poverty and social inequality on TB transmission. Additionally, the COVID-19 pandemic has further strained healthcare systems, leading to disruptions in TB services.
![[History of Accounting SS1]: A Journey Through the Evolution of Financial Practices history-of-accounting-ss1_2](https://www.lolaapp.com/wp-content/uploads/2023/12/history-of-accounting-ss1_2-150x150.jpg)