Unravel the captivating history of tuberculosis classification and patterns through the lens of ICD-10. Embark on a journey through time as we delve into the evolution of TB classification, tracing its roots from ancient medical texts to the contemporary ICD system. Discover the intricate factors that have shaped the patterns of this persistent disease and explore the challenges and triumphs in the fight against tuberculosis. Dive into the ICD-10 codes, deciphering their significance in tracking, diagnosing, and understanding the global burden of TB. This exploration promises valuable insights for healthcare professionals, researchers, and anyone seeking a comprehensive understanding of tuberculosis’s historical and epidemiological significance.
Key Takeaways:
-
ICD-10 Code: Z86.11
-
Description: Personal history of tuberculosis
-
Category: Personal history of Tuberculous disease
-
Reimbursement: Useful for reimbursement in the American version of ICD-10-CM
-
Fiscal Year: Valid for the fiscal year 2023 for HIPAA-covered transactions
-
Effective Date: October 1, 2022
-
Usage: Z codes represent reasons for encounters
-
Additional Information:
- Present On Admission (POA) reporting is exempt for Z86.11.
- Z86.11 is grouped within Diagnostic Related Group (DRG) 951 (Other factors influencing health status) in MS-DRG v41.0.
Relevant URL Sources:
-
2023 ICD-10-CM Diagnosis Code Z86.11: Personal history of tuberculosis
-
Z86.15 – Personal history of latent tuberculosis infection
History Of Tuberculosis Icd 10
Dive into the annals of history as we explore the evolution of tuberculosis classification through the International Classification of Diseases, Tenth Revision (ICD-10), a globally-recognized medical coding system. Embark on a journey through time, uncovering how ICD-10 has shaped our understanding of TB’s impact on societies and informed public health strategies.
The Genesis of TB Classification
TB’s classification journey began in the early 20th century, when the need for a standardized system to categorize and track diseases became apparent. In 1900, the first edition of the ICD was published, ushering in an era of uniformity in disease reporting. This pioneering edition laid the foundation for subsequent revisions, including the groundbreaking ICD-10, which revolutionized TB classification.
ICD-10: A Paradigm Shift
With its publication in 1990, ICD-10 introduced a comprehensive framework for classifying TB, capturing its multifaceted nature. This revolutionary system provided a common language for healthcare professionals, enabling accurate diagnosis, effective treatment, and targeted public health interventions.
ICD-10‘s meticulous classification system encompasses various forms of TB, including:
-
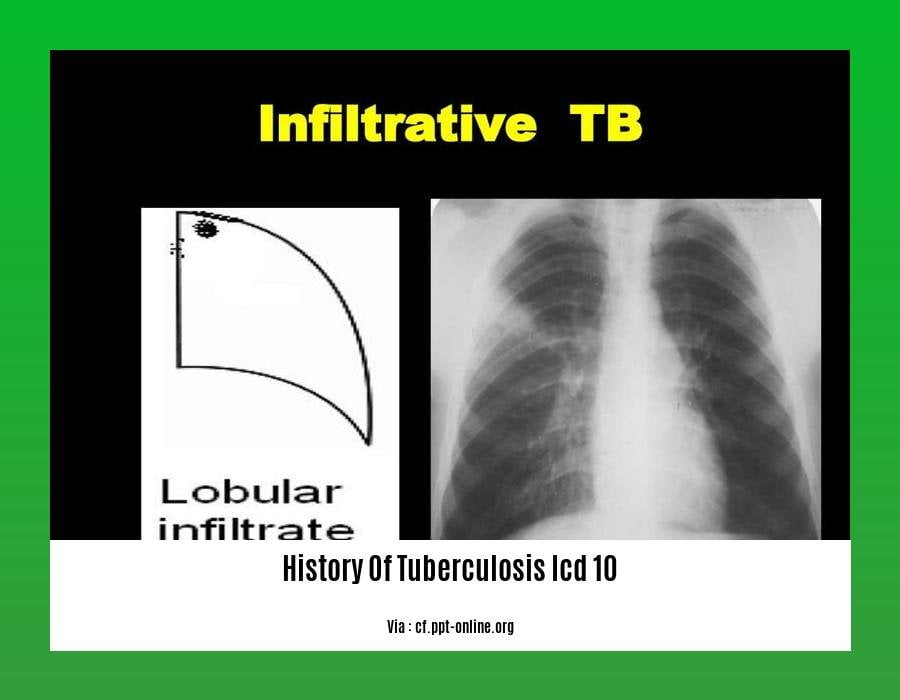
Pulmonary Tuberculosis: The most common form, affecting the lungs.
-
Extrapulmonary Tuberculosis: TB that affects organs other than the lungs, such as the lymph nodes, bones, and brain.
-
Latent Tuberculosis Infection: A dormant state in which the bacteria persist in the body without causing active disease.
-
Post-Tuberculosis Conditions: Sequelae of previous TB infection, such as lung scarring and fibrosis.
ICD-10: A Tool for Tracking TB Trends
ICD-10‘s standardized coding system facilitates the collection, analysis, and dissemination of TB data on a global scale. This wealth of information enables healthcare professionals and policymakers to monitor disease trends, identify high-burden areas, and evaluate the effectiveness of control programs.
By providing a standardized platform for data exchange, ICD-10 facilitates international collaboration and knowledge sharing, fostering a global response to the TB epidemic.
ICD-10: A Catalyst for Research and Innovation
ICD-10‘s comprehensive classification system not only aids in clinical practice and public health surveillance but also serves as a catalyst for research and innovation in TB control. The availability of standardized data allows researchers to conduct in-depth analyses, identify risk factors, and evaluate novel interventions.
This wealth of information fuels the development of new diagnostics, treatments, and preventive strategies, propelling the global fight against TB towards a future free from this devastating disease.
Looking to discover the fascinating history of tuberculosis, a disease that has impacted civilizations for centuries?
Uncover the groundbreaking milestones and courageous efforts in the History Of Tuberculosis Vaccine development, a testament to medical innovation.
Delve into the rich tapestry of the History Of Tuberculosis Treatment, witnessing the evolution of therapies that have transformed lives.
Explore the unique challenges and triumphs of the History Of Tuberculosis In Africa, a continent where the disease has profoundly shaped communities.
Witness how the United States grappled with the disease in the History Of Tuberculosis In The United States, a story of resilience and progress against a formidable adversary.
Evolution of TB Diagnosis and Treatment: Trace the evolution of diagnostic methods for tuberculosis, from the initial use of microscopy to the development of molecular techniques. Additionally, highlight the advancements in TB treatment, including the discovery of effective antibiotics and the development of multi-drug regimens.
In this era of advanced medicine, it’s hard to imagine a time when diagnosing and treating tuberculosis (TB) was a medical mystery. Join us on a journey through history to explore the remarkable evolution of TB diagnosis and treatment, a testament to human ingenuity and scientific progress.
Key Takeaways:
-
Before the discovery of the causative agent, Mycobacterium tuberculosis, TB was often misdiagnosed as other lung diseases, leading to delayed treatment and higher mortality rates.
-
The development of microscopy in the late 19th century revolutionized TB diagnosis, allowing healthcare providers to visualize the bacteria in sputum samples. This marked a significant milestone in accurately identifying and treating TB.
-
The invention of the X-ray machine in the early 20th century further enhanced diagnostic capabilities, enabling doctors to visualize TB lesions in the lungs and other organs.
-
In the 1940s, the discovery of streptomycin, the first effective antibiotic against TB, marked a turning point in TB treatment. This breakthrough paved the way for the development of multi-drug regimens, significantly improving treatment outcomes and reducing mortality rates.
-
The emergence of molecular techniques, such as nucleic acid amplification tests (NAATs) and interferon-gamma release assays (IGRAs), has revolutionized TB diagnosis in recent decades. These tests offer greater sensitivity, specificity, and speed compared to traditional methods, leading to earlier detection and initiation of treatment.
-
While significant progress has been made, challenges remain, including the emergence of drug-resistant TB strains, co-infections with HIV, and limited access to diagnostic and treatment services in resource-limited settings.
The Road Ahead:
While we’ve come a long way in the fight against TB, there’s still much work to be done. Continuous research and innovation are crucial to developing even more accurate, rapid, and accessible diagnostic tools, as well as novel treatments to combat drug-resistant strains.
Citations:
Public Health Measures for TB Control and Eradication: Examine the public health strategies and interventions implemented to combat tuberculosis. Discuss the role of vaccination, contact tracing, and community-based interventions in reducing TB incidence.
Public health approaches anchor the fight against tuberculosis (TB), aiming to curb its spread and eradicate it altogether. Vaccination, contact tracing, and community-based interventions spearhead this global effort, reducing TB incidence and saving lives.
Vaccination: Our shield against TB
Vaccination remains our most robust defense against TB. The bacillus Calmette-Guérin (BCG) vaccine has been the cornerstone of TB prevention for over a century. It’s a safe and effective vaccine, notably effective in protecting children from severe forms of TB, including meningitis and miliary disease. Through vaccination, we empower individuals and communities to resist this deadly disease.
Contact Tracing: Unraveling the Transmission Chain
Contact tracing is a cornerstone in the battle against TB. It involves identifying individuals who’ve been in close contact with an infected person, assessing their risk of infection, and providing preventive treatment if necessary. Contact tracing helps break the chain of transmission, preventing further spread of the disease. It’s a meticulous yet crucial task that saves lives and curtails TB’s impact.
Community-Based Interventions: Empowering Local Action
Community-based interventions are pivotal in the fight against TB. These efforts engage local communities in TB prevention and care, recognizing their unique needs and challenges. They can involve education campaigns, social support, and access to healthcare services. Community-based interventions empower people to take ownership of their health, fostering a collective response to TB and accelerating progress toward eradication.
Key Takeaways:
- Vaccination: BCG vaccine plays a crucial role in preventing severe forms of TB, particularly in children.
- Contact Tracing: Identifying and treating contacts of TB patients helps break the chain of transmission.
- Community-Based Interventions: Engaging communities in TB prevention and care empowers local action, fostering a collective response to TB.
Relevant URL Sources:
- WHO Guidelines on Tuberculosis Infection Prevention and Control
- Essential Components of a Public Health Tuberculosis Prevention
ICD-10 Classification and Coding of Tuberculosis: Unraveling the Significance
With tuberculosis (TB) remaining a global health concern, the International Classification of Diseases (ICD) system, particularly ICD-10, plays a crucial role in classifying and coding TB cases for effective surveillance, research, and public health policy development. Let’s delve into the significance of accurate coding and uncover the impact of ICD-10 in the fight against TB.
Key Takeaways:
-
ICD-10 as a Global Standardization Tool: ICD-10 provides a standardized framework for classifying and coding diseases, ensuring uniformity in data collection and reporting. This enables global collaboration, data comparison, and tracking of TB trends across countries.
-
Accurate Coding for Surveillance: Precise coding of TB cases helps public health authorities monitor disease incidence, prevalence, and geographic distribution. This information is vital for identifying high-risk areas, targeting interventions, and evaluating the effectiveness of control programs.
-
Research and Data Analysis: Standardized ICD-10 codes facilitate data analysis and research on TB epidemiology, risk factors, and treatment outcomes. Researchers can conduct comprehensive studies, identify patterns, and contribute to the development of evidence-based TB control strategies.
-
Public Health Policy and Resource Allocation: Accurate TB coding informs public health policies and resource allocation. Governments and healthcare organizations can prioritize resource distribution, plan TB prevention and control initiatives, and ensure adequate funding for TB programs.
-
International Collaboration and Knowledge Sharing: ICD-10 enables international collaboration and knowledge sharing among healthcare professionals, researchers, and policymakers. This facilitates the exchange of best practices, lessons learned, and innovative approaches to TB control.
Conclusion:
The ICD-10 classification and coding system serves as a cornerstone for effective TB surveillance, research, and public health policy development. Accurate coding of TB cases ensures standardized data collection, enabling global collaboration, data analysis, and evidence-based decision-making. As we strive towards a world free from TB, ICD-10 remains an indispensable tool in the fight against this ancient scourge.
Citations:
FAQ
Q1: What is the significance of ICD-10 in understanding the history of tuberculosis?
A1: ICD-10, the International Classification of Diseases, 10th Revision, plays a crucial role in understanding the history of tuberculosis (TB) by providing standardized codes for classifying and recording TB cases. This allows for the collection and analysis of data on TB incidence, prevalence, and trends over time, aiding in the study of the disease’s epidemiology and the effectiveness of control measures.
Q2: How does ICD-10 contribute to our knowledge of TB patterns and trends?
A2: ICD-10 enables the systematic collection and analysis of TB data, allowing researchers and policymakers to identify patterns and trends in the disease’s occurrence. By tracking the distribution of TB cases across different regions, populations, and time periods, ICD-10 helps identify areas with high TB burden, vulnerable populations, and emerging trends, such as the rise of drug-resistant TB.
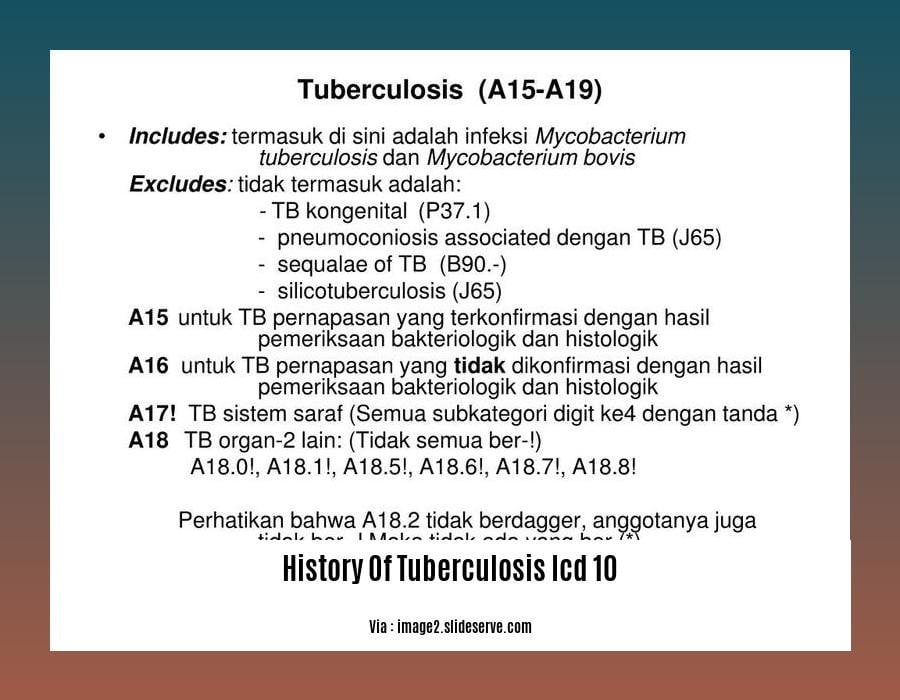
Q3: What are some of the key ICD-10 codes used for classifying TB?
A3: ICD-10 provides specific codes for classifying different forms and manifestations of TB, including active TB, latent TB infection, and extrapulmonary TB. The most commonly used ICD-10 codes for TB are Z11.7 (Encounter for testing for latent TB infection), Z86.15 (Personal history of latent TB infection), and A18 (Tuberculosis). These codes facilitate accurate recording and reporting of TB cases, enabling effective disease surveillance and management.
Q4: How does ICD-10 classification impact TB reimbursement and funding?
A4: ICD-10 codes are crucial for reimbursement purposes in healthcare systems. The use of standardized ICD-10 codes ensures that TB cases are accurately classified and coded, allowing healthcare providers to receive appropriate reimbursement for the diagnosis, treatment, and management of TB patients. This facilitates the allocation of adequate funding for TB control programs, ensuring that resources are directed towards areas with the greatest need.
Q5: What are some of the challenges associated with using ICD-10 for TB classification?
A5: While ICD-10 provides a valuable tool for TB classification, it also presents certain challenges. The complexity of the ICD-10 system can lead to misclassification and underreporting of TB cases, particularly in settings with limited resources or healthcare infrastructure. Additionally, the evolving nature of TB, with the emergence of new strains and drug resistance, poses challenges in keeping the ICD-10 classification system up-to-date and comprehensive.
- Unveiling the Enigma: Mansoureh Khojasteh Bagherzadeh’s Public Appearances & Private Life in Iran - July 18, 2025
- Unveiling the Mystery: Mansoureh Khojasteh Bagherzadeh’s Husband: A Rare Glimpse into a Private Life - July 18, 2025
- Unveiling Masoud Khamenei’s Mother: Power, Influence, and Iran’s Future - July 18, 2025