Dive into the remarkable history of preterm delivery in [- The History of Preterm Delivery: A Journey of Discovery and Advancements]. From its humble beginnings to the cutting-edge treatments of today, this article chronicles the fascinating evolution of preterm birth care, showcasing the challenges and triumphs that have shaped the field.
Key Takeaways:
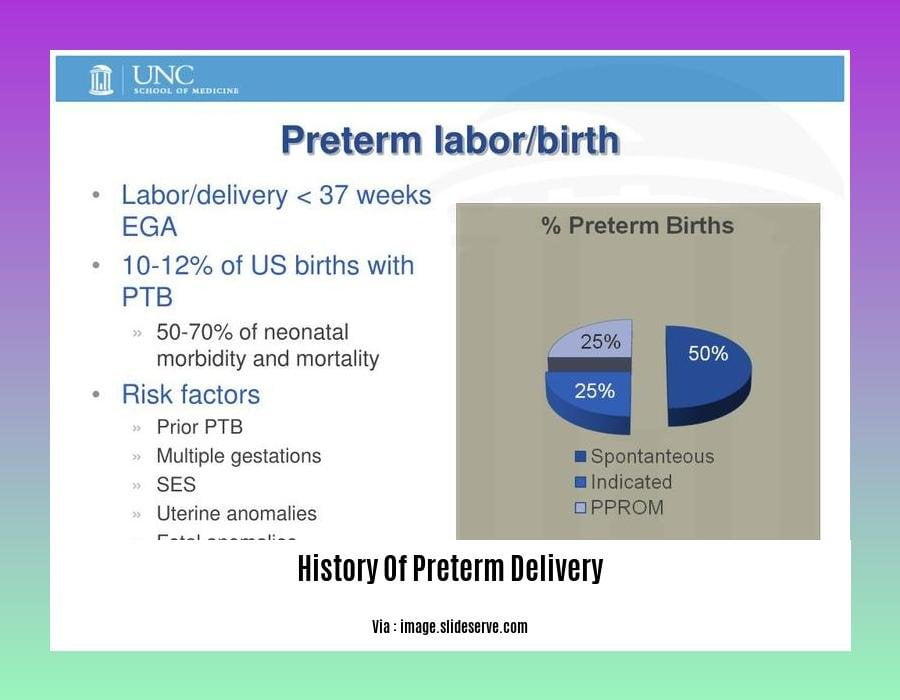
- Preterm birth occurs before 37 weeks of pregnancy.
- The majority of causes for prematurity are unknown.
- Medical conditions and certain factors can contribute to premature birth.
- Preterm labor is classified into two types: spontaneous and medically induced.
- The global rate of premature birth varies from 4% to 16%.
- Asia and sub-Saharan Africa have the highest rates of premature births.
History Of Preterm Delivery
Throughout history, preterm delivery has been a prevalent issue in maternal and child health, with babies born before the completion of 37 weeks of pregnancy facing various challenges.
Ancient Beliefs and Practices
In ancient times, preterm birth was often associated with supernatural forces or divine intervention. Traditional practices and beliefs varied across cultures, with some resorting to rituals or sacrifices to prevent premature deliveries.
Medical Advancements in the 18th and 19th Centuries
The 18th and 19th centuries witnessed significant advancements in medical knowledge and practices. Physicians began to recognize the importance of prenatal care and hygiene, making strides in identifying potential risk factors for preterm delivery.
20th Century: Identifying Causes and Treatments
The 20th century brought groundbreaking discoveries in the field of preterm birth. Researchers identified specific causes, such as infections, placental abnormalities, and premature rupture of membranes. Simultaneously, the development of incubators and neonatal intensive care units (NICUs) improved the survival rates of premature infants.
Modern Era: Innovations and Challenges
In the modern era, continued research and technological advancements have led to further improvements in preterm birth care. Non-invasive prenatal testing has enhanced the early detection of risk factors, while advancements in fetal monitoring and labor management have contributed to more precise interventions.
Despite these advancements, preterm delivery remains a global issue, with significant regional variations in rates and outcomes. Ongoing research focuses on understanding the intricate mechanisms underlying preterm labor, exploring preventive measures, and optimizing care for both mothers and infants.
Looking Ahead: Hope for the Future
The History Of Preterm Delivery is marked by both triumphs and challenges. However, the ongoing dedication of healthcare professionals, researchers, and advocates gives hope for a future where preterm birth is prevented, and every baby has the opportunity to thrive.
If you’re looking to uncover the history of preterm birth care, our comprehensive article delves into the evolution of care for premature infants, tracing advancements from the early days to modern practices.
For a deeper understanding of the History Of Preterm Birth, explore our article that unveils the complex factors contributing to preterm delivery and the ongoing efforts to reduce its incidence.
Expecting mothers with a History Of Preterm Delivery Currently Pregnant can find invaluable guidance in our article, which offers tailored advice and support to navigate the challenges and ensure a healthy pregnancy.
If you’re concerned about Family History Of Preterm Labor, our article provides insights into the genetic and environmental influences that may increase the risk and offers practical steps to mitigate potential complications.
Our article on the History Of Preterm Labor provides a thorough account of the causes and consequences of premature labor, highlighting the importance of early detection and intervention strategies.
Challenges and Controversies: Ethical and Social Dilemmas
Neonatal intensive care units (NICUs) grapple with ethical quandaries daily. These dilemmas often revolve around life-sustaining treatments for infants with low birth weights.
Key Considerations
Informed Consent: Obtaining consent from parents is crucial, but it can be challenging when decisions involve complex medical interventions with uncertain outcomes.
Balancing Benefits and Burdens: Weighing potential benefits against the possible burdens of treatment requires a nuanced approach that considers the infant’s long-term well-being.
Conflicts with Parents: Differences in perspectives between parents and healthcare providers can create ethical conflicts. Open communication and shared decision-making are essential.
Ethical Principles
Four ethical principles guide decision-making in NICUs:
- Autonomy: Respecting parents’ rights to participate in decisions.
- Beneficence: Acting in the best interests of the infant.
- Non-maleficence: Avoiding harm and minimizing suffering.
- Justice: Ensuring equitable access to care and resources.
Key Takeaways:
- Ethical dilemmas in NICUs involve decisions about life-sustaining treatments for very low birth weight infants.
- Informed consent, balancing benefits and burdens, and resolving conflicts between parents and healthcare providers are key ethical considerations.
- The ethical principles of autonomy, beneficence, non-maleficence, and justice guide decision-making.
- Open communication, shared decision-making, and respect for parental rights are essential in navigating ethical dilemmas in NICUs.
Relevant URL Sources:
- Ethical Issues in Treating Infants With Very Low Birth Weights
- Ethical Dilemmas in the Care of Preterm Infants
The Preterm Spectrum: Variations in Gestational Age and Outcomes
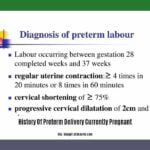
Understanding the profound impact of the preterm spectrum requires delving into the variations in gestational age and their associated outcomes. Preterm birth, before the magical 37th week of pregnancy, encompasses three distinct categories: extreme preterm, very preterm, and preterm.
Gestational Age and Preterm Birth Categories
| Gestational Age | Type of Preterm Birth |
|---|---|
| Before 28 weeks | Extreme Preterm Birth |
| 28-32 weeks | Very Preterm Birth |
| 32-37 weeks | Preterm Birth |
The Preterm Spectrum: Challenges and Risks
The preterm spectrum presents a cascade of challenges for both the tiniest patients and their families. Premature infants are more vulnerable to a multitude of complications, ranging from respiratory distress syndrome to neurological impairments. The younger the gestational age, the greater the risk of severe long-term health issues.
Key Takeaways:
- Preterm birth: Occurs before 37 weeks of gestation.
- Variations in gestational age: Extreme preterm, very preterm, and preterm birth.
- Higher risks: Preterm infants face elevated health risks, with extreme preterm births posing the greatest challenges.
- Gestational age: A critical factor in determining the severity of preterm birth outcomes.
Shaping the Future of Preterm Care
While the preterm spectrum poses significant challenges, relentless advancement in medical technology and research offer hope. Embracing the power of collaboration, researchers and healthcare providers strive to unravel the complexities of preterm birth and improve outcomes for these vulnerable infants and their families.
Relevant URL Sources
- Preterm Birth: Causes, Consequences, and Prevention
- The Preterm Spectrum: A Global Perspective
Current Landscape and Future Directions: Innovations and Ongoing Research
Today, the field of preterm birth care is characterized by an array of cutting-edge advancements and ongoing research initiatives that are revolutionizing the way we prevent, diagnose, and treat this multifaceted condition.
Innovations that are Reshaping Preterm Birth Care:
- Non-invasive prenatal testing: Allows early detection of genetic abnormalities that may increase the risk of preterm birth.
- Advanced fetal monitoring: Continuous monitoring of fetal heart rate and movement patterns provides early warning signs of potential complications.
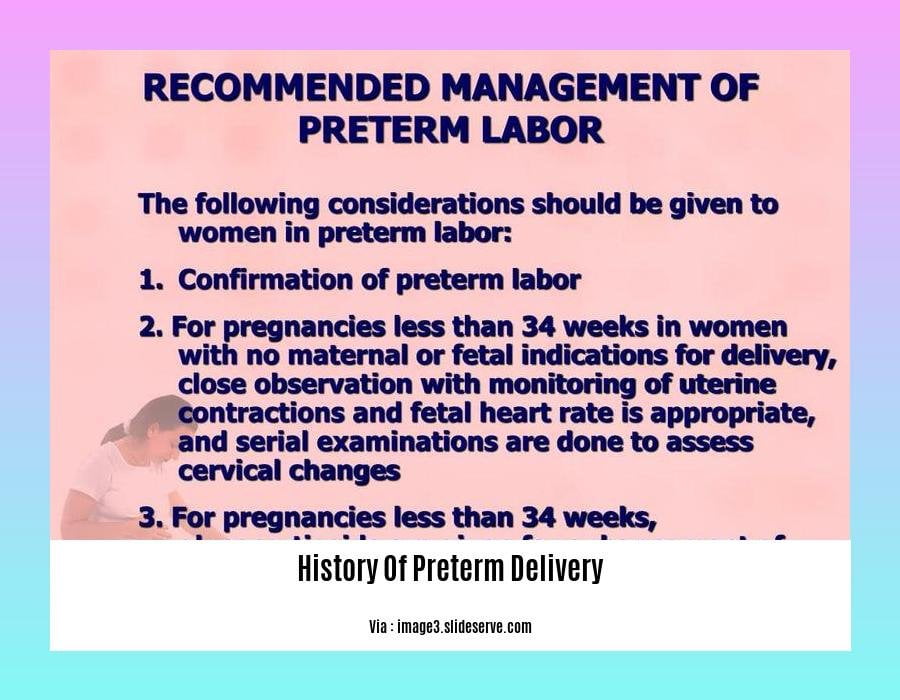
- Targeted labor management: Precise interventions like cervical cerclage and progesterone therapy are tailored to individual risk profiles, reducing preterm birth rates.
Research Efforts Guiding the Future:
- Identification of risk factors: Ongoing studies aim to identify modifiable risk factors, such as maternal health conditions and lifestyle choices, that contribute to preterm birth.
- Early detection and prevention strategies: Research focuses on developing reliable biomarkers and screening tools to detect women at risk of preterm birth early in pregnancy.
- Improved treatments for preterm infants: Innovations in neonatal care, including advancements in respiratory support, nutrition, and infection control, are improving the outcomes of premature babies.
Key Takeaways:
- Innovations like non-invasive prenatal testing and advanced fetal monitoring are revolutionizing preterm birth care.
- Research efforts are focused on identifying risk factors, developing early detection strategies, and improving treatments for preterm infants.
- The future of preterm birth care holds promise for reducing rates and improving outcomes through ongoing research and innovation.
Relevant URL Sources:
- Future Directions in Preterm Birth Research
- Landscape of Preterm Birth Therapeutics and a Path Forward