Discover the evolution of preterm delivery management in [A Historical Perspective on Preterm Delivery: Implications for Current Pregnancy]. Healthcare professionals are invited to delve into the historical context and its profound impact on contemporary approaches to ensuring optimal outcomes for women and their families.
Key Takeaways:
- Preterm birth is a major global concern, accounting for 10% of all births.
- Causes are complex and involve medical, psychosocial, and biological factors.
- Known risk factors include:
- Previous preterm birth
- Maternal age (younger than 17 or older than 35)
- Multiple pregnancy
- Uterine abnormalities
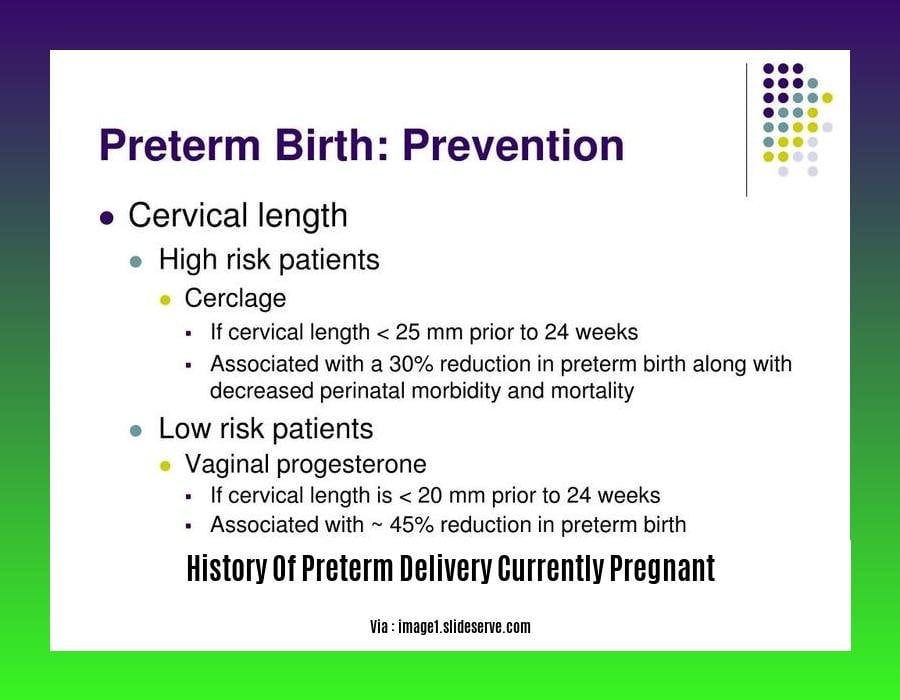
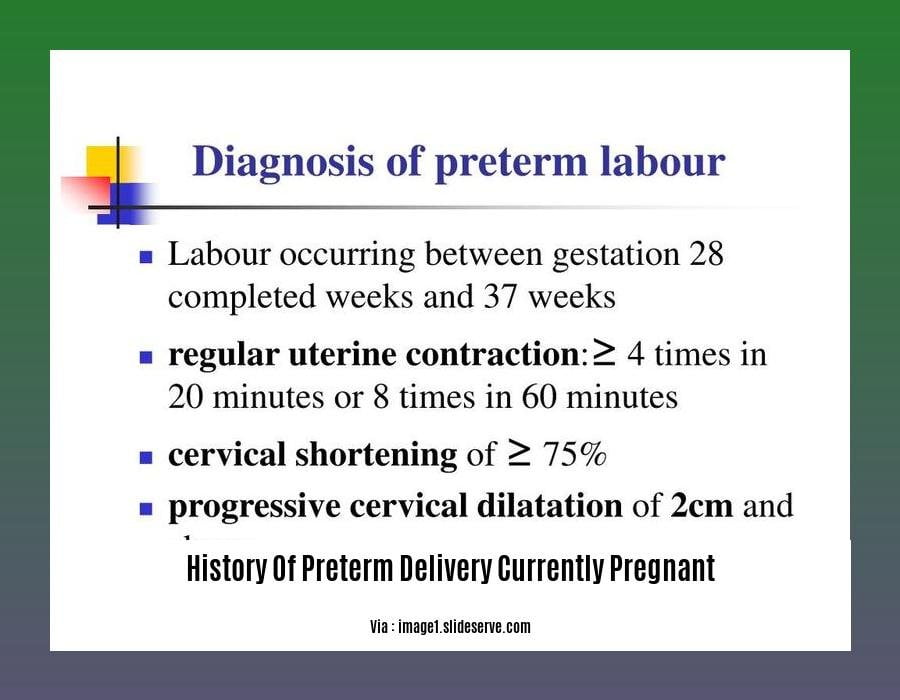
- Prediction is challenging but certain factors can indicate higher likelihood:
- Short cervix
- Fetal fibronectin in cervical secretions
- Positive stress test
- Family history
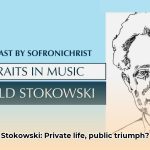
- Predicting preterm birth allows for early intervention and management:
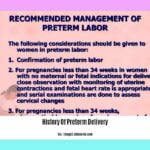
- Tocolysis to stop contractions
- Maternal corticosteroids to promote fetal lung development
- Magnesium sulfate for brain protection
- Hospitalization for monitoring
History Of Preterm Delivery Currently Pregnant
The history of preterm delivery is a complex one, with evidence of premature births dating back to ancient times. Hippocrates, the father of Western medicine, described infants born before their time as “weak and sickly.” In the 16th and 17th centuries, premature infants were often baptized immediately after birth, as they were not expected to survive long.
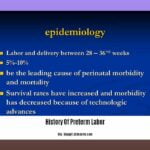
The first successful attempts to save the lives of premature infants were made in the 19th century, with the development of incubators and other life-saving technologies. However, it was not until the 20th century that preterm birth began to be recognized as a major public health problem. In the 1950s, the World Health Organization (WHO) defined preterm birth as the delivery of a baby before the completion of 37 weeks of gestation.
Today, preterm birth remains a significant global health concern, accounting for approximately 10% of all births worldwide. It is the leading cause of neonatal mortality and morbidity, and can have long-term consequences for the health and development of children.
Preterm birth is a complex condition with multiple causes, including:
Medical causes:
- Infections
- Uterine abnormalities
- Placental problems
- Preeclampsia
- Gestational diabetes
Behavioral causes:
- Smoking
- Alcohol use
- Drug use
- Poor nutrition
- Stress
Social causes:
- Poverty
- Lack of access to healthcare
- Domestic violence
The risk of preterm birth is also higher for certain groups of women, including:
- Women who are pregnant for the first time
- Women who are under 17 or over 35 years old
- Women who have had a previous preterm birth
- Women who are carrying multiples
- Women who have certain medical conditions, such as diabetes or high blood pressure
Preterm birth can be prevented in some cases, but there is no surefire way to prevent it. However, there are a number of things that women can do to reduce their risk, including:
- Getting regular prenatal care
- Eating a healthy diet
- Maintaining a healthy weight
- Avoiding smoking, alcohol, and drugs
- Managing stress
- Getting enough sleep
If you are currently pregnant and concerned about your risk of preterm birth, talk to your doctor. There are a number of things that your doctor can do to help you reduce your risk and improve your chances of having a healthy baby.
Do you want to know more about the history of preterm birth? Learn more about the history of preterm birth care to gain an understanding of the evolution of its management strategies over time. Dive deeper into the history of preterm birth to uncover the key milestones and advancements in the field. Explore the history of preterm delivery to gain insights into the historical perspectives on preterm birth management. For a comprehensive understanding of the genetic aspects, delve into the family history of preterm labor. And lastly, shed light on the history of preterm labor to gain valuable knowledge about its origins and impact on pregnancy outcomes.
Consequences and complications of preterm birth for the mother and infant
Consequences for Infants:
- Respiratory Distress Syndrome: Underdeveloped lungs make breathing difficult.
- Chronic Lung Disease: Persistent lung inflammation and scarring.
- Injury to the Intestines: Necrotizing enterocolitis, a life-threatening condition.
- Neurological Impairment: Cerebral palsy, developmental delay, learning disabilities.
Consequences for Mothers:
- Increased Risk of Postpartum Hemorrhage: Excessive bleeding after delivery.
- Infection: Higher risk of chorioamnionitis and endometritis.
- Preeclampsia: A serious pregnancy complication characterized by high blood pressure and protein in the urine.
- Long-Term Health Issues: Increased risk of cardiovascular disease, diabetes, and certain cancers later in life.
Key Takeaways:
- Preterm birth is associated with a range of health risks for both mothers and infants.
- Consequences for infants include respiratory distress syndrome, chronic lung disease, intestinal injury, and neurological impairment.
- Mothers face an increased risk of postpartum hemorrhage, infection, preeclampsia, and long-term health issues such as cardiovascular disease and diabetes.
- Understanding these risks is crucial for informed decision-making and optimal care during preterm deliveries.
References:
– Mortality and Acute Complications in Preterm Infants
– Epidemiology and causes of preterm birth
Current Best Practices and Medical Interventions for Managing Preterm Birth
Since its recognition centuries ago, preterm birth has puzzled medical practitioners. In the past, newborns born prematurely faced a bleak outlook, with survival rates being particularly low. Fortunately, technological advancements, particularly in the 19th century, have significantly improved the chances of these fragile infants.
Contemporary Approaches to Preterm Birth Management
In today’s medical landscape, we are armed with a more refined understanding of preterm delivery, allowing for more effective management:
Antenatal Corticosteroids: These medications trigger fetal maturity, reducing the risk of preterm birth by enhancing lung development and other vital functions.
Cervical Cerclage: In cases of cervical weakness, surgical reinforcement can prevent premature dilation and subsequent preterm labor.
Uterine Rest and Lifestyle Modifications: Bed rest, limited physical activity, and avoiding stress can contribute to maintaining a stable pregnancy and reducing the likelihood of preterm birth.
The choice of optimal intervention is individualized and guided by factors such as the mother’s medical history, the stage of pregnancy, and the baby’s condition.
Key Takeaways:
- Antenatal corticosteroids enhance fetal maturity, reducing the risk of preterm birth.
- Cervical cerclage offers surgical support to weak cervixes, preventing premature dilation.
- Uterine rest, limited physical activity, and stress management promote pregnancy stability.
Relevant URL Sources:
- Preventing Preterm Birth: Next Generation Strategies
- WHO Recommendations on Interventions to Improve Preterm Birth Outcomes
Ongoing Research and Future Prospects in Preterm Birth Prevention and Management
Key Takeaways:
– Globally, 15 million infants are born prematurely, with an increased risk of health complications.
– PTB is a leading cause of neonatal mortality and morbidity.
– Only one FDA-approved therapy exists for PTB prevention in the US.
Ongoing Research
Researchers are exploring various avenues to prevent and manage preterm birth, including:
- Identification of risk factors: Better understanding of maternal, fetal, and environmental factors associated with PTB can improve screening and targeted interventions.
- Novel therapies: Developing new medications and interventions to inhibit preterm labor and promote fetal maturity.
- Personalized medicine: Utilizing genetic and molecular markers to tailor PTB prevention and management strategies to individual patients.
Future Prospects
Advances in technology and scientific understanding hold promise for improving preterm birth outcomes:
- Advanced fetal monitoring: Non-invasive techniques to monitor fetal well-being and identify early signs of labor.
- Artificial intelligence (AI): AI algorithms can analyze large datasets to predict preterm birth risk and guide personalized care.
- Stem cell therapy: Potential for repairing damaged fetal membranes or promoting cervical ripening.
Collaboration and Innovation
Collaboration among researchers, healthcare providers, and policymakers is crucial to translate ongoing research into tangible improvements for women and their babies. Investment in research and innovation will pave the way for a future where preterm birth is significantly reduced and the health and well-being of premature infants are enhanced.
Relevant URL Sources:
- Preventing Preterm Birth: Next Generation Strategies by Hannah C. Zierden et al.
- WHO Recommendations on Interventions to Improve Preterm Birth Outcomes by World Health Organization

![[History of Accounting SS1]: A Journey Through the Evolution of Financial Practices history-of-accounting-ss1_2](https://www.lolaapp.com/wp-content/uploads/2023/12/history-of-accounting-ss1_2-150x150.jpg)