Imagine a medical procedure so groundbreaking it won a Nobel Prize, yet so devastating it’s now considered a medical nightmare. That’s the story of the prefrontal lobotomy. This isn’t just a dry history lesson; it’s a wild ride through the highs and lows of a procedure that promised a cure for mental illness but delivered a whole lot of unintended, and often horrific, consequences. We’ll meet the doctors, driven by good intentions but tragically misguided, and the patients, whose lives were forever altered. We’ll see how a procedure that initially offered hope quickly spiraled out of control, fueled by hype and a lack of understanding. This is the story of how a medical miracle turned into a cautionary tale, a stark reminder of the importance of ethical considerations in medical advancement. For another example of tragically misguided medical practices, read about Ignaz Semmelweis’s struggles.
The History of Lobotomy: A Nobel Prize-Winning Medical Nightmare & Brain Surgery Advancements
The story of the lobotomy is a strange and unsettling one – a tale of a medical procedure that won a Nobel Prize, yet left a trail of devastated lives in its wake. It’s a reminder that even groundbreaking medical advancements can go horribly wrong, highlighting the critical importance of careful research, ethical considerations, and a healthy dose of skepticism. Did this Nobel Prize validation lead to premature adoption and overlook potential long-term damages?
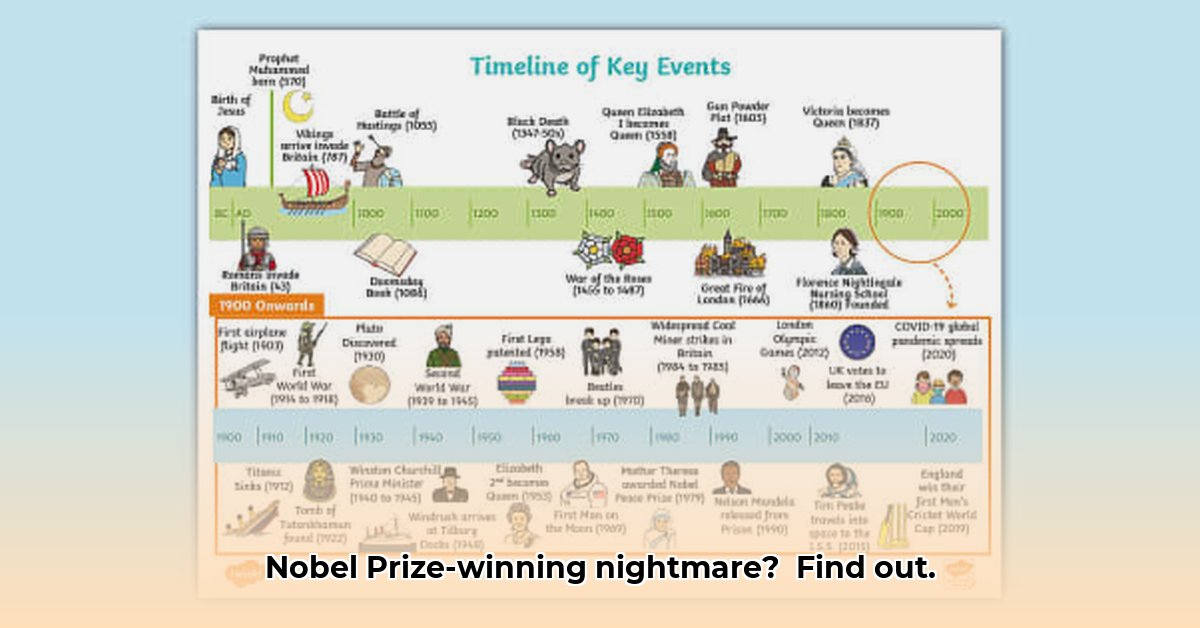
The saga begins in the 1930s with António Egas Moniz, a Portuguese doctor. He devised a procedure called prefrontal leucotomy (essentially severing connections in the brain’s front part). Moniz believed this could magically cure severe mental illnesses like schizophrenia, severe depression, and anxiety disorders. Amazingly, he won the Nobel Prize in Medicine in 1949 for his work. But looking back, was this a medical triumph, or a horrific mistake? The truth, as we’ll uncover, is far more complicated.
Initially, some patients did seem to improve. Their agitation calmed down; some symptoms eased. At the time, mental hospitals were overflowing, and desperate people and doctors desperately needed effective treatments. This initial, limited success, fueled the procedure’s rapid rise in popularity. However, doctors often overlooked, or maybe downplayed, major negative side effects. Serious problems like apathy, drastic personality shifts, profound cognitive impairment, and even death, weren’t always fully reported or discussed openly. Some patients were left in a vegetative state, unable to care for themselves, while others experienced seizures and other neurological complications.
Things took a darker turn with the arrival of the transorbital lobotomy in the 1940s. American doctor Walter Freeman popularized a much simpler version – the “ice pick lobotomy.” It involved inserting an ice pick-like instrument through the eye socket! It was quicker, less invasive (relatively speaking!), and could be done in minutes. Freeman even traveled the country, performing lobotomies in traveling shows and demonstrating the procedure to large audiences. This ease of use, unfortunately, meant it was often performed with very little assessment or follow-up of patients. Did these patients truly understand the risks involved? Were they truly giving their informed consent, or were these invasive procedures administered without adequate consideration of their rights? These ethical questions remain troubling, even today. Consider the case of Rosemary Kennedy, sister of President John F. Kennedy, who underwent a lobotomy at the age of 23 and was left permanently incapacitated.
By the 1950s, a new wave of treatments emerged – powerful antipsychotic drugs like chlorpromazine. These drugs offered a less invasive and often reversible way to help those struggling with mental illness. The lobotomy’s popularity swiftly plummeted. Later, long-term studies revealed the true devastating impact on the lives of those who underwent the procedure. The initial excitement and hope quickly gave way to deep regret and a profound sense of loss for patients and their families.
The legacy of the lobotomy stands as a sobering reminder of the importance of several key aspects of medical practice. First, it underscores the need for rigorous, long-term research before widely adopting novel medical procedures. Researchers need to look at short-term effects; they need to understand the long-term consequences. Second, ethical review and truly informed consent are absolutely crucial. Patients have the right to know the full picture, including potential risks, before undergoing potentially life-altering procedures. Finally, the story highlights the critical need for responsible and balanced information sharing, both among medical professionals and the wider public.
The lobotomy’s story isn’t just a tale of medical mishaps; it’s a potent cautionary tale. It’s a story about the complex interplay of hope, innovation, and ethical responsibility in medicine – a balancing act we must continually strive to get right.
A Summary of Key Issues Affecting the Lobtomies’ Success and Ethical Concerns
Consider these pivotal issues that impacted the lobotomy’s initial success and the subsequent ethical quandaries:
- Initial Apparent Success: Short-term improvements in some patients led to optimism and acceptance despite limited evidence. This is a critical factor that must be looked upon in long-term research.
- Simplified Procedure Hazards: The transorbital approach, while less invasive initially, increased risks due to simplicity and lack of precision. The relative ease of the ice-pick lobotomy led to it being rapidly and, in retrospect, recklessly adopted.
- Lack of Long-Term Research: Early adoption ignored potential for severe long-term disabilities and negative consequences. What if longitudinal studies had been rigorously performed before widespread adoption?
| Aspect | Description | Impact |
|---|---|---|
| Initial Apparent Success | Some patients showed short-term improvements in symptoms, creating an initial wave of optimism and widespread acceptance despite limited evidence. | This fueled widespread adoption despite the lack of long-term data and a complete understanding of potential risks. |
| Simplified Procedure Hazards | The transorbital (“ice pick”) approach, while less invasive initially, increased the risk of severe side effects due to its simplicity and lack of precision. | This exacerbated negative results and raised significant ethical concerns about informed consent and acceptable medical standards. |
| Lack of Long-Term Research | Early adoption relied on limited data, ignoring the potential for severe long-term disabilities and negative consequences for patients. | Many patients suffered irreversible harm, leaving a legacy of regret and questioning within the medical community. |
| Ethical Concerns & Consent | Questionable informed consent practices, combined with the irreversible nature of the procedure, raised serious ethical questions. | This led to widespread controversy concerning the autonomy of the patient and the limits of medical intervention. |
| Pharmacotherapy’s Rise | The development of antipsychotic medications provided less invasive and often reversible treatment options. | This led to the rapid decline of lobotomies as safer and more effective treatments became available. |
| Societal Context | Overcrowded mental institutions and a lack of alternative treatments created a desperate search for solutions. | This desperation contributed to the acceptance of a risky procedure with limited evidence of long-term efficacy. |
The history of the lobotomy serves as a powerful lesson. It forces us to continually re-evaluate how we approach medical innovation, ensuring that the pursuit of progress doesn’t come at the cost of patient welfare and ethical considerations. It is a story we must never forget.
How Did Media Portrayal Influence Lobotomy’s Adoption and Ethical Controversies? & Media Influence on Public Health
The story of the prefrontal lobotomy is a chilling example of how medical innovation, amplified by media, can lead to widespread adoption despite questionable efficacy and significant ethical concerns. Initially, the procedure—involving severing connections in the brain’s frontal lobe—was presented as a miracle cure for a range of mental illnesses. But how did this portrayal shape its rapid adoption and subsequent downfall? Does the media have a responsibility to temper excitement with critical analysis in medical reporting?
A Media-Fueled Miracle?
Early media coverage, particularly in some countries like Sweden and the United States, often painted a rosy picture. Articles highlighted successful cases, showcasing patients’ transformation from violent or severely disturbed individuals to calmer, more manageable ones. These stories often focused on the relief experienced by families and caregivers, further amplifying the perceived benefits of the procedure. This positive framing fueled optimism among both the public and medical professionals. The apparent simplicity of the procedure—compared to other treatments available at the time—also contributed to its appeal. Did this enthusiastic media coverage overshadow the potential risks? Newspapers and magazines lacked the critical perspective and detailed reporting that we expect today. The lack of rigorous scientific evidence to support the procedure’s effectiveness was largely ignored. It was a time when the line between hope and hype was easily blurred. This positive narrative contributed significantly to the procedure’s rapid adoption across multiple countries in the mid-20th century. Some reports even romanticized the procedure, portraying doctors as heroic figures battling against the scourge of mental illness.
The Shadow Side: Unseen Risks and Ethical Lapses
Slowly but surely, the dark side of the lobotomy began to emerge. Initial reports of high mortality rates and severe side effects—including personality changes, intellectual impairment, and emotional blunting—were initially downplayed or dismissed in some media. However, as more cases emerged, so did the ethical questions. The lack of informed consent—a now-fundamental aspect of medical ethics—was commonplace. Patients, often desperate or lacking agency, were subjected to the procedure without a full understanding of the risks involved. Ethical lapses and the unforeseen consequences: How did the media address this growing conflict between the initial hype and the grim reality? The response varied considerably across nations. Some publications began to publish stories of patients who had been negatively affected by lobotomies, highlighting the devastating consequences of the procedure. An unbiased reporting practice can save lives.
The discrepancy between the positive initial media coverage and the subsequent revelations of widespread side effects and mortality serves as a cautionary tale. The story of lobotomy highlights the potential for media bias to influence medical decision-making, both on the level of individual patients and wider societal acceptance of a medical procedure.
A Global Perspective: Contrasting Narratives
The reception of lobotomy varied across nations. While some countries like Sweden saw initially positive media coverage that fueled widespread adoption, the American experience shows a different dynamic, reflecting a complex interplay of media influence, medical practice, and regulatory oversight (or the lack thereof). In the Soviet Union, the lobotomy was banned in 1950 due to its perceived inhumanity and lack of scientific basis.
Comparative studies of media reporting in different countries reveal strikingly different narratives surrounding the lobotomy’s introduction, adoption, and ultimate decline. These differences highlight the importance of considering cultural and societal contexts when evaluating the role of media in shaping medical practices.
The Legacy of the “Miracle Cure”
The history of psychosurgery, specifically the widespread practice of lobotomy, offers a stark reminder of the importance of rigorous scientific scrutiny, ethical considerations, and balanced media reporting in the adoption of any novel medical procedure. The initial enthusiasm, amplified by media, ultimately led to a widespread tragedy. The story of the lobotomy remains a crucial case study in medical ethics and the dangers of unchecked technological advancement. This case highlights the media’s crucial role in public health.
Key Takeaways:
- The early portrayal of lobotomy in the media was overwhelmingly positive. What consequences resulted from this enthusiasm?
- This positive media coverage played a significant role in the procedure’s widespread adoption. Why was there so little discussion of the risks?
- The lack of rigorous scientific evidence was overlooked in the initial wave of enthusiasm.
- Subsequent revelations of high mortality rates and debilitating side effects were initially downplayed or ignored.
- Ethical concerns regarding informed consent were largely absent in the early years.
- Cross-national comparisons reveal variations in media responses and the subsequent regulation of the procedure.
- The lobotomy’s legacy provides cautionary insights into medical innovation, media influence, and ethical responsibility.
- The media should strive to present a balanced view of medical advancements, highlighting both potential benefits and risks.
Media Portrayal and Public Perception of Lobotomy Procedures & Psychology and Society
Key Takeaways:
- The initial media portrayal of lobotomies was overwhelmingly positive, fueling public enthusiasm and contributing to the procedure’s widespread adoption. How did the media influence public perception?
- This positive public perception, however, masked significant risks and negative consequences for patients.
- The stark contrast between initial hype and later recognition of devastating outcomes reveals the pitfalls of unchecked medical innovation and the power of media portrayal in shaping medical practices. What can the media do to more responsibly cover medical procedures?
- Variations in media portrayal and regulatory oversight between countries (like the US and Sweden) led to differing rates of adoption and ultimately, different outcomes.
The “Miracle Cure” Takes Center Stage
Imagine a time when mental illness was shrouded in mystery. Treatments were often crude, effectiveness questionable. Then came the lobotomy, presented as a revolutionary solution. Early media portrayal often depicted it as a miracle cure, capable of transforming violent or severely disturbed patients into calm, functional individuals. Newsreels, magazine articles, and even fictional accounts spun tales of dramatic recoveries. This enthusiastic media portrayal fueled public demand, and soon, lobotomies were the latest “must-have” treatment. Was this a realistic view? The media often focused on the positive outcomes while downplaying the potential risks and long-term consequences.
A Closer Look at the Procedure
The lobotomy itself varied over time, from the more invasive prefrontal lobotomy to the quicker, less precise transorbital approach popularized by Walter Freeman. Freeman’s technique — inserting an ice pick-like instrument through the eye socket — shocked and intrigued some, even earning him the label of “the lobotomist.” This dramatic image became part of the procedure’s growing notoriety. While some early reports were positive, the long-term consequences of destroying brain tissue were often horrific: personality changes, apathy, seizures, incontinence, and even death.
In fact, a history journal notes this about Walter Freeman’s famous “ice pick” lobotomy: inserting an ice pick-like instrument through the patient’s eye socket [1]
The Shift in Public Opinion
The initial positive media portrayal gave way to a more critical view as the devastating effects of lobotomies became undeniable. As more cases of severe complications emerged, so did skepticism among medical professionals. The rise of effective psychopharmacological treatments further cemented the decline in popularity of lobotomies. The negative consequences significantly altered the public perception, transforming it from one of enthusiastic acceptance to deep caution. Ethical standards in psychology and society must evolve with new technological developments, as demonstrated by the consequences of public perception of the lobotomy. The story of the lobotomy is a cautionary tale of overblown promises and the ethical challenges inherent in medical innovation. Films like “One Flew Over the Cuckoo’s Nest” further contributed to the growing public awareness of the potential dangers of lobotomies.
Comparing Approaches: US vs. Sweden
While the US saw a widespread adoption of lobotomies, fueled by the positive early media portrayal, other countries had different experiences. Sweden, for instance, also performed thousands of lobotomies, but the media portrayal and overall enthusiasm were less extreme, not as openly celebratory. The lack of stringent oversight and the involvement of general surgeons rather than specialists contributed to a higher initial mortality rate, further impacting the public perception. This international comparison underscores the significant role of both media portrayal and regulatory oversight in shaping medical practices and patient outcomes.
A Legacy of Ethical Questions
The history of lobotomies isn’t just a narrative of medical innovation gone wrong; it’s a powerful case study in ethical considerations. The initial excitement overshadowed a proper evaluation of the procedure’s risks and long-term consequences. The lobotomy serves as a reminder of the importance of rigorous scientific testing, careful consideration of ethical implications, and balanced media portrayal in the development and implementation of any medical intervention. The procedure’s legacy continues to prompt discussions about informed consent, the vulnerability of patients, and the power of media portrayals to shape public opinion on complex medical issues. Does this history give you pause and make you think about how we approach medical advancements today? The story of Rosemary Kennedy, and her tragic outcome after undergoing a lobotomy, also contributed to the growing public awareness of the procedure’s potential dangers.
Ethical Considerations in Early Lobotomy Procedures and Informed Consent & History of Medical Ethics
Key Takeaways:
- The prefrontal lobotomy, initially lauded, became a medical cautionary tale. What lessons can be learned from its history?
- Its widespread use stemmed from societal pressures, questionable ethics, and a lack of rigorous testing.
- Ethical Considerations in Early Lobotomy Procedures and Informed Consent were severely lacking. What impact did that have on patients?
- The procedure’s legacy highlights the urgent need for stringent ethical guidelines and robust research.
The Rise of a “Miracle Cure”
Imagine a time when mental illness was poorly understood, stigmatized, and often left untreated. Overcrowded asylums were commonplace, and desperate families sought any solution for their loved ones’ suffering. Into this landscape arrived the prefrontal lobotomy, initially hailed as a groundbreaking treatment. Egas Moniz, its pioneer, even received a Nobel Prize. However, this seemingly revolutionary procedure carried a dark side, one that raises profound questions about Ethical Considerations in Early Lobotomy Procedures and Informed Consent.
A Surgical Gamble: The Procedure and its Consequences
Lobotomy involved severing connections in the brain’s prefrontal cortex. While initially showing promise in reducing agitation, the long-term consequences were often catastrophic. Patients frequently suffered severe personality changes, cognitive impairments, emotional blunting, and even death. The procedure was undeniably invasive, irreversible, and far riskier than initially believed. What ethical concerns were raised by early psychiatric researchers’ practices? The lack of understanding of the brain and the long-term effects of severing neural connections contributed to the ethical concerns.
The Transorbital Approach: A Simpler, Yet More Dangerous Method
Walter Freeman II, a prominent American neurologist, further popularized a particularly controversial technique: the transorbital lobotomy. This involved inserting an ice pick-like instrument through the patient’s eye socket, a far less precise, and far more dangerous, approach with even higher chances of irreversible damage. Freeman traveled the country performing these procedures, sometimes in front of large audiences, further contributing to the ethical concerns surrounding the procedure.
A Crisis of Consent: The Ethical Failures
Many patients underwent lobotomies without truly understanding the procedure’s risks or even explicitly consenting. This represents a major failure of Ethical Considerations in Early Lobotomy Procedures and Informed Consent. Institutionalized patients, particularly, lacked the agency to make independent choices. The power imbalance between doctors and patients was stark, creating a system where vulnerable individuals were subjected to risky procedures without their informed consent. In many cases, family members made the decision on behalf of the patient, without fully understanding the potential consequences.
The Media’s Role: Hype and Subsequent Backlash
Early media portrayals often sensationalized lobotomy’s supposed benefits, creating a perception of a quick and easy fix for intractable mental illness. This fueled the procedure’s widespread adoption, despite its questionable efficacy and substantial risks. However, as the devastating long-term consequences became clear, public opinion shifted, exposing the inherent ethical failures and leading to a justified backlash. The media’s initial positive portrayal contributed to the lack of critical evaluation of the procedure’s risks.
The Fall from Grace: The Rise of Psychopharmacology
The advent of psychopharmacology, with the development of antipsychotic drugs, delivered a more effective and less invasive approach to mental illness treatment. As safer and more effective options emerged, the popularity of lobotomy plummeted. This shift marked a crucial turning point in the history of psychiatry, underscoring the critical need for rigorous scientific evaluation and ethical considerations in medical practice.
Lessons Learned: The Enduring Significance
The history of lobotomy serves as a stark reminder of the potential dangers of unchecked medical innovation and the imperative of Ethical Considerations in Early Lobotomy Procedures and Informed Consent. It highlights the critical need for robust ethical guidelines, thorough research, and transparent, unbiased information dissemination, particularly when dealing with vulnerable populations. The story of lobotomy remains a cautionary tale, shaping ethical discussions in medical practice to this day. The legacy of the lobotomy continues to inform discussions about patient rights, informed consent, and the ethical responsibilities of medical professionals.
- Understand the Dunning-Kruger Effect: Why Incompetent People Think They’re Experts: Gain Self-Awareness - August 1, 2025
- Ignaz Semmelweis: The Doctor Fired for Handwashing: A Public Health Tragedy - August 1, 2025
- Unlock Your Memory: Spaced Repetition: The Scientific Trick to Remembering Information Forever: Learn Effortlessly - August 1, 2025