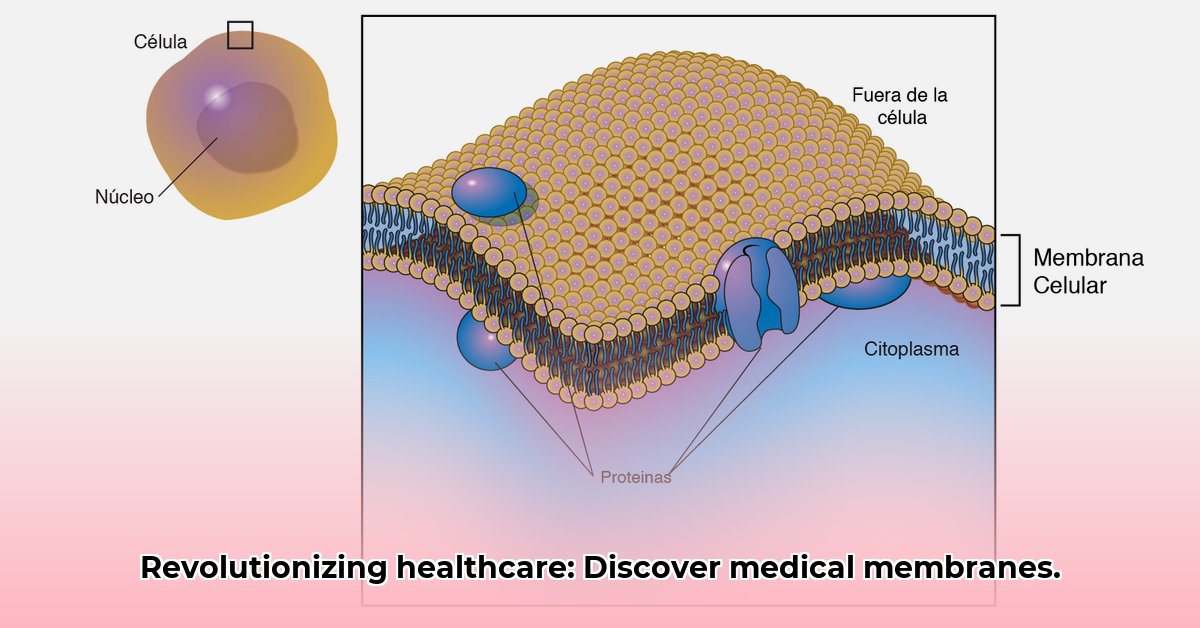
Imagine tiny, super-efficient filters working inside the human body – that’s essentially what medical membranes are. These thin layers of material perform a crucial role in healthcare, from life-saving dialysis to targeted drug delivery. For more on innovative medical technologies, check out this resource. This article explores the science behind these membranes, explaining how they work, the types available, and their importance in modern medicine. We’ll also examine the latest advancements, showcasing how researchers are expanding the possibilities for treating diseases with these innovative filters.
The Revolution of Medical Membrane Technology
Medical membranes – thin, selective barriers – are transforming healthcare. They are integrated into devices such as dialysis machines and drug delivery systems. Advances in material science, the need for minimally invasive procedures, and a deeper understanding of how membranes interact with the human body have led to their increasing use.
Understanding Medical Membranes
Medical membrane technology is advancing rapidly. Microfiltration and ultrafiltration techniques are complemented by specialized membranes used in hemodialysis, blood purification, and targeted drug delivery. The challenge lies in developing membranes that are effective and safe for the human body, biocompatible, resistant to bodily fluids, and selective in what they allow to pass through.
Key Characteristics of Medical Membranes
Several characteristics define a successful medical membrane:
-
Selective Permeability: Membranes must selectively allow certain substances to pass through while blocking others, enabling the separation of toxins from the blood or the delivery of drugs to specific cells.
-
Biocompatibility: Compatibility with the body is essential to avoid triggering immune responses or rejection, especially for long-term implants.
-
Chemical Resistance: Membranes must withstand exposure to bodily fluids, digestive acids, and sterilization chemicals without degrading.
-
Durability: A long lifespan is necessary for cost-effectiveness and ensuring consistent membrane performance over time.
Applications in Healthcare
Medical membranes are used in critical healthcare applications:
-
Hemodialysis: Membranes act as artificial kidneys in dialysis machines, removing waste products from the blood for patients with kidney failure.
-
Blood Oxygenation: In heart-lung machines used during cardiac surgeries, membranes oxygenate the blood and remove carbon dioxide. 3M™ MEMBRANA OXYPLUS capillary membrane systems are used to enable effective blood oxygenation in patients with respiratory conditions.
-
Therapeutic Apheresis: Specialized membrane systems selectively remove harmful components, such as antibodies or excess cholesterol, from the blood. 3M’s capillary membranes for therapeutic apheresis are crafted using synthetic polymers, ensuring the efficient removal of harmful components from the blood or plasma while preserving essential blood components.
-
Drug Delivery: Membranes encapsulate drugs and release them precisely where needed, enhancing effectiveness and reducing side effects.
Challenges and Solutions
Despite advancements, challenges remain in the medical membrane field:
-
Regulatory Approval: Obtaining approval for new medical membrane devices requires rigorous testing and data to demonstrate safety and efficacy. Streamlined approval processes are needed to accelerate innovation.
-
Cost Reduction: Reducing the cost of manufacturing is crucial for making these technologies accessible. Efficient production methods and affordable materials are key.
-
Standardization: Consistent standards in manufacturing, testing, and implementation are needed to accelerate progress.
Advances in Membrane Technology
The field of medical membranes is poised for continued growth and innovation:
-
New Materials: Scientists are developing new materials with improved properties, leading to more effective, durable, and biocompatible membranes.
-
Personalized Medicine: Membrane designs can be tailored to individual patient needs, optimizing treatment effectiveness and minimizing adverse reactions.
-
Integration with Other Technologies: Membranes are being integrated with technologies like organ-on-a-chip systems for drug testing and microfluidic devices for fluid management.
Actionable Steps for Progress
To fully exploit the potential of medical membranes, a collaborative effort is necessary:
| Stakeholder | Short-Term Actions (0-1 Year) | Long-Term Actions (3-5 Years) |
|---|---|---|
| Manufacturers | Optimize manufacturing, reduce costs, invest in biomaterial research, improve quality control. | Develop next-generation membranes with enhanced performance, explore new manufacturing techniques. |
| Medical Device Companies | Rigorous testing and evaluation, collaborate on new designs, meet regulatory standards. | Invest in R&D, integrate membranes with advanced medical technologies, simplify the scale-up process, ensure regulatory standards. |
| Regulatory Agencies | Streamline approvals, maintain safety, develop standardization guidelines. | Establish international standards for testing and approval, promote adoption and innovation. |
| Healthcare Providers | Implement new technologies after evaluation and training, gather performance data, reach out to experts to discuss further. | Training programs on advancements, participate in research collaborations. |
The field of medical membranes is at a pivotal point. With collaborative efforts addressing the remaining challenges, the potential to transform healthcare is within reach.
Hemodialysis Membrane Comparison: Balancing Cost and Efficacy
Key Takeaways:
- High-cutoff (HCO) membranes show potential benefits for patients with cast nephropathy, but more research is needed.
- High-flux membranes improve dialysis adequacy (KT/V), but their impact on removing mid-sized molecules is debated.
- Expanded hemodialysis (HDx) may be cost-effective in the long run due to reduced hospital readmissions.
- Membrane selection depends on individual patient needs.
- Large-scale clinical trials are crucial for definitive comparisons.
Hemodialysis Membrane Types
Hemodialysis relies on membranes to filter blood, but not all membranes are equal. Comparing the cost and effectiveness of different types is crucial for optimizing patient care.
High-Cutoff (HCO) Membranes
HCO membranes have larger pores, allowing for the removal of larger molecules. While some studies suggest improved outcomes in conditions like cast nephropathy, more conclusive evidence is needed.
High-Flux vs. Low-Flux Membranes
High-flux membranes enhance dialysis adequacy. However, their efficacy in removing mid-sized molecules is debated.
Expanded Hemodialysis (HDx)
HDx, using advanced membranes, may offer long-term savings through reduced hospitalizations and improved patient quality of life.
Biocompatibility
Membrane biocompatibility influences patient outcomes and safety by minimizing adverse reactions.
Data Gaps, Individualized Care and Membranes
Large-scale, randomized controlled trials are needed to compare membrane types definitively. The ideal membrane depends on individual patient characteristics and disease severity.
Membrana™ SYNPHAN™ capillary membranes find application across various treatment modes, including hemodialysis, hemodiafiltration, hemofiltration, and hemoconcentration.
- Understand the Dunning-Kruger Effect: Why Incompetent People Think They’re Experts: Gain Self-Awareness - August 1, 2025
- Ignaz Semmelweis: The Doctor Fired for Handwashing: A Public Health Tragedy - August 1, 2025
- Unlock Your Memory: Spaced Repetition: The Scientific Trick to Remembering Information Forever: Learn Effortlessly - August 1, 2025