Imagine being able to provide life-saving breaths to someone struggling to breathe. Bag-mask ventilation (BMV) empowers you to do just that. This guide equips you with the techniques and knowledge to master BMV and deliver this critical procedure confidently.
Understanding Bag-Mask Ventilation
Bag-mask ventilation is a manual way to deliver breaths to someone who isn’t breathing or isn’t breathing effectively. It’s like manually breathing for them until professional help arrives or their breathing improves. This technique involves using a bag-valve-mask (BVM) device to push air, often enriched with oxygen, into a person’s lungs. If you are planning a boat trip, you must be aware of your alcohol use while operating or being a passenger.
How BMV Works
The BVM setup consists of a self-inflating bag, a one-way valve, a face mask, and an optional oxygen reservoir. Squeezing the bag forces air through the one-way valve, preventing backflow. The mask creates a seal over the person’s nose and mouth, directing the airflow into their lungs. The reservoir, if used, connects to an oxygen source, delivering highly oxygenated breaths.
Key Points for Using a Bag-Mask Device:
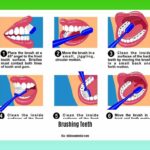
Initial Setup: Ensure an open airway by positioning the head in a neutral or slightly tilted-back position. Select the right mask size for a snug fit over the nose and mouth. If available, connect the oxygen reservoir and set the appropriate flow rate (usually 10-15 liters per minute).
Mask Placement: Gently place the mask over the face, using the “E-C clamp” technique to create an airtight seal. This involves shaping your thumb and index finger like a “C” around the mask, while your other fingers lift the jaw into an “E” position.
Ventilation Technique: Squeeze the self-inflating bag smoothly and steadily over one second, aiming to deliver a tidal volume of approximately 500 mL for an average adult. Observe for chest rise, confirming breath delivery. Allow the bag to refill completely before the next squeeze.
Ventilation Rate & Monitoring: Ventilate adults at a rate of 1 breath every 5-6 seconds (10-12 breaths/minute). Children and infants require different rates; consult updated guidelines from organizations like the American Heart Association (AHA). Monitor chest rise and fall and use a pulse oximeter if available to track oxygen saturation levels.
Two-Rescuer Ventilation (Optimal Method): One rescuer maintains a proper mask seal and airway patency, while the other rescuer squeezes the bag rhythmically.
Troubleshooting:
- Mask Leaks: Check the seal, ensure the mask is the right size, and reposition. Lubricating the mask’s edges may improve the seal and patient comfort.
- Inadequate Chest Rise: Verify a clear airway, carefully increase bag pressure (while remaining gentle), or slightly adjust the head angle. An oropharyngeal or nasopharyngeal airway may be helpful if advanced training allows.
- Gastric Distension (Air in Stomach): Adjust the head angle, ensure appropriate ventilation pressure and technique, consider inserting an orogastric tube (with appropriate training).
Delivering Effective Breaths
Ventilation Rates
The ideal ventilation rate and volume are still under investigation. While 10-12 breaths per minute is the current guideline for adults, some research suggests that lower rates may be beneficial in certain situations. Other research focuses on using tidal volume monitoring to personalize ventilation. The AHA provides specific recommendations for children and infants which should always be consulted. Ongoing research suggests that real-time feedback, such as oxygen saturation and capnography, may help refine ventilation strategies.
Technique Refinements
Beyond the basics, proper BMV technique involves consistently delivering the correct tidal volume (about 500 mL for adults), smooth and controlled bag compressions, careful observation of chest rise, and ongoing assessment of the patient’s condition. Current research explores the effects of various mask designs and ventilation techniques on patient outcomes. For instance, newer BVM designs incorporate PEEP valves, allowing clinicians to maintain positive end-expiratory pressure, which can be beneficial in certain respiratory conditions. These areas of ongoing research highlight the dynamic nature of medical best practice.
Two-Person BVM
Two-person BVM is the optimal method, as one person focuses on mask seal and airway maintenance, while the other delivers the breaths. This teamwork maximizes ventilation efficiency, especially in challenging situations. It also minimizes fatigue, which can compromise the quality of ventilations over extended periods. Consistent communication between the two rescuers is essential for coordinated and effective BVM.
Advanced Considerations and Potential Complications
Advanced Airway Management
In some cases, advanced airway management techniques like intubation may be necessary. While beyond the scope of this guide, it’s important to recognize that BVM often serves as a bridge to these more definitive airway interventions. Training in advanced techniques is crucial for healthcare professionals managing complex airway scenarios.
Potential Complications
Even with correct technique, complications can arise. Gastric inflation (air entering the stomach) can occur, especially if the mask seal isn’t perfect or if excessive pressure is used. Barotrauma (lung injury from too much pressure) is another potential risk. While rare, these complications underscore the importance of proper training and ongoing vigilance while performing BMV. Hypoxia (low oxygen levels), while a reason to initiate BMV, can also persist if ventilation is ineffective. Continuous monitoring and adjustment of technique are essential.
Additional Tips and Training
While this guide provides valuable information, hands-on training from qualified instructors is essential to develop proficiency in BMV. Simulated scenarios, practice on manikins, and regular refreshers are crucial for maintaining skills and confidence. Local protocols and guidelines should always be followed. Furthermore, understanding the psychological impact of performing BVM is important. The stress of an emergency situation can affect both the rescuer and the patient’s family. Communicating calmly and clearly can help alleviate anxiety and promote a sense of control.
This information is intended for educational purposes only and is not a substitute for professional medical advice. Always consult with a healthcare professional for any concerns about a medical condition.













1 thought on “Bag-Mask Ventilation: A Practical Guide to Delivering Rescue Breaths”
Comments are closed.